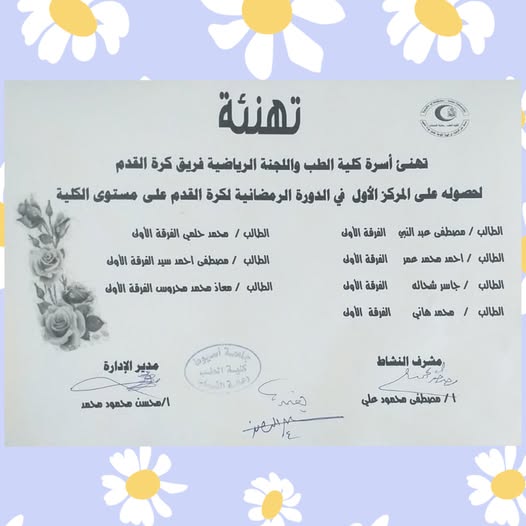
The Faculty of Medicine and the Sports Committee congratulate the Faculty of Medicine football team.
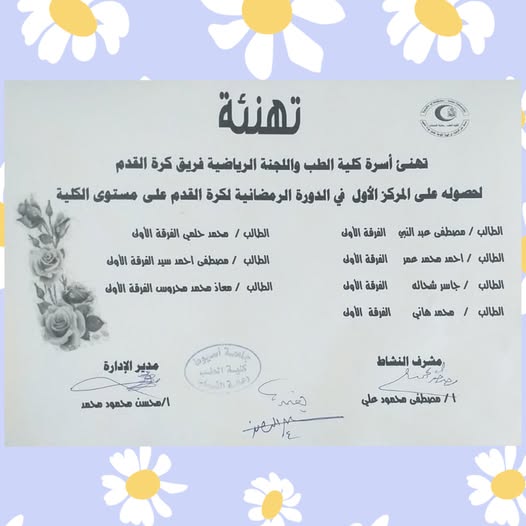
The Faculty of Medicine and the Sports Committee congratulate the Faculty of Medicine football team.




Background
Juvenile idiopathic arthritis (JIA) is an autoimmune, inflammatory noninfective joint disease that includes different disease subtypes that are characterized by the onset of arthritis starting before the age of 16 years with symptoms lasting at least for 6 weeks.
Objective
The aim of this study was to evaluate the compliance of healthcare providers at the Pediatric Rheumatology Unit, Assiut University Children’s Hospital, to the 2011 American College of Rheumatology recommendations for treatment of JIA.
Patients and methods
The study was conducted on 50 patients who were younger than 16 years and diagnosed as having JIA at the Pediatric Rheumatology Unit, Assiut University Children’s Hospital, to assess compliance of the unit’s healthcare providers to American College of Rheumatology recommendations for treatment of JIA.
Results
The patients were grouped according to age into two groups: from 1 to 7 and 8 to 16 years. Polyarticular JIA was the most common type among studied cases followed by systemic‑onset JIA. All studied cases presented with arthritis at the time of diagnosis. Complete blood count and erythrocyte sedimentation rate were done for all studied cases at the time of diagnosis. Rheumatoid factor was done for 84%. The most common complications among the studied group were those related to treatment. NSAIDs and corticosteroids were the most common drugs used.
Conclusion
Treatment of JIA includes pharmacological and nonpharmacological interventions and surgical treatment. Pharmacological treatment includes NSAIDs, steroids, disease‑modifying antirheumatic drugs, and biological agents. The degree of disease activity and the presence or absence of features of poor prognosis greatly affect onset of complications and treatment of JIA. Nonpharmacological interventions include psychosocial therapy, nutrition, physical and occupational therapy, lifestyle factors, and home remedies. Through this study, some defects were found. First, there was deficiency in data recording. Second, there was also deficiency in laboratory (mainly rheumatoid factor and antinuclear antibody/anti‑double stranded DNA) and radiological workup. Moreover, nonpharmacological therapy and surgery were not considered. Lastly, there was deficiency in regular follow‑up of safety drug monitoring.
Background: The shortage of healthcare professionals, coupled with the expansion of health services, has made Community Health Workers (CHWs) an effective solution to bridge these gaps. The objective was to determine the actual employed services of CHWs in the health system with especial emphasis on their role in family planning services. Methods: A cross-sectional study was conducted among 250 CHWs from Assiut governorate using a self-administered questionnaire about sociodemographic and job characteristics together with roles and tasks performed by CHWs. Results: All CHWs in the study were female, with 51.2% being under 40 years old and 82% were recruited by the Ministry of Health and Population. CHWs primarily served mothers and children (99.2%) and were involved in health education (100%), puerperium care (99.2%), family planning (98.8%), pregnancy (97.6%) and breastfeeding (96%). They also participated in health initiatives like family planning (98.8%) and maternal and childcare (92.4%). The most common health issue observed by CHWs was chronic diseases (73.2%), while non-medical concerns included poverty (78.4%) and unemployment (78.4%). Conclusion and recommendation: CHWs offer a wide range of health services, provide health education, and actively participate in various health initiatives. The study emphasized the crucial role of CHWs in strengthening health systems, particularly in rural areas, by enhancing both coverage and quality of services. It is essential for health system stakeholders to focus on developing a training program matching a clear job description to ensure that CHWs can maximize their impact in meeting community health needs.
Background: Diabetes distress (DD) is a significant barrier to effective self-care and diabetes management. This study aimed to evaluate the frequency of DD among patients with diabetes at Assuit University Hospital (AUH) and identify potential predictors. Additionally, to explore the relationship between DD and diabetes-related stigma, and self-care activities.
Methods: A cross-sectional study was conducted with 295 patients with diabetes at AUH. Data were collected using questionnaires on sociodemographic and clinical characteristics, DD, diabetes-related stigma, and self-care activities.
Results: The average age of the patients was 53.9±9.6 years, with the majority being female (85.5%). The mean duration of diabetes was 9.34±5.7 years. About two-thirds of the patients had uncontrolled diabetes (67.1%). Nearly half (47.8%) of participants experienced moderate to high levels of DD, while 52.2% reported little or no DD. The highest level of DD was regimen-related among 49.5% and the lowest was emotional burden among 13.6%. Statistically significant associations were found between DD and factors such as age, marital status, treatment type, hypertension, nephropathy, HbA1c levels, and stigma scale. In the adjusted logistic regression model, the predictors of moderate or high levels of DD included being 40-60 years, married, hypertensive, having nephropathy, experiencing a high level of stigma, and having elevated HbA1c levels.
Conclusions: High degree of DD was found to be linked with high levels of HA1c level and a higher perception of diabetes-related stigma. Screening for DD, and diabetic stigma together with tailoring self-care activities should be principal components of diabetes management protocols.
Uveitis is a major cause of visual impairment. Most uveitis cases have autoimmune etiology. Pediatric autoimmune uveitis may be associated with systemic diseases such as juvenile idiopathic arthritis or may arise as an isolated disorder. It may be accompanied by retinal vasculitis due to retinal microcirculation involvement. Nailfold capillaroscopy, a digital microscope, is a non-invasive tool for systemic microcirculation evaluation. We aimed to evaluate systemic microcirculation abnormalities in pediatric autoimmune uveitis. Twenty-five patients with pediatric autoimmune uveitis and 21 healthy children underwent detailed capillaroscopic evaluation. We assessed capillary density/mm, capillary morphology, capillary dimensions, and the presence or absence of microhemorrhages and avascular areas. The mean age of the study and control groups was 11.24 ± 3.03 and 9.9 ± 4.17 years, respectively. Most …
Objectives
We aimed to analyze auditory involvement in patients with Behcet’s disease and its association with Optical Coherence Tomography Angiography findings and disease manifestations.
Methods
This study included 54 eyes and 68 ears of 34 adults with Behcet’s disease in comparison to 30 eyes and 60 ears of healthy controls. Clinical, laboratory and ophthalmological evaluation including Optical Coherence Tomography Angiography was done. Audiological assessment included otoscopic examination, immitancemetry and pure tone and speech audiometry.
Results
Sensorineural hearing loss was observed in 32.35% of the studied cases. Behcet’s disease patients showed significantly higher average hearing level and significant reduction of retinal vessel density compared to controls. Patients with sensorineural hearing loss demonstrated significantly lower central retinal capillary vessel density and higher …

