Subjective and functional outcome measures to evaluate performance of pediatric cochlear implant
The Role of Non-Invasive Ventilation (NIV) In the Era of COVID-19 Pandemic
MINI REVIEW With the current emergent situation of Coronavirus disease-19 (COVID-19) pandemic all over the world, the need for ventilators increases every day. About 1-3% of COVID-19 patients can develop acute respiratory distress syndrome (ARDS) that ranges from mild to severe [1]. So, the shortage of mechanical ventilators is expected to be a critical problem in many countries. Non-invasive ventilation (NIV) may help in the Management of COVID-19 patients. It does not replace invasive mechanical ventilation but can provide a bridge to it [2]. In China, more than 50% of treated patients required NIV or High Flow Nasal Cannula [3]. However, the World Health Organization (WHO) reported NIV as a high-risk aerosolgenerating procedure, increasing the risk of infection transmission, especially to healthcare providers [4].
Clinical outcome of 1-year long-term oxygen therapy in patients with chronic obstructive pulmonary disease
Hemostasis in Thyroidectomy comparison between diathermy and ligasure
Effect of non-alcoholic fatty liver disease on outcome of primary pci in non-diabetic stemi patients
The effect of Non-alcoholic fatty liver disease (NAFLD) on outcome of patients with ST- segment elevation myocardial infarction (STEMI) is controversial. The purpose of the study aimed to assess the effect of non-alcoholic fatty liver disease (NAFLD) on myocardial and epicardial reperfusion after primary percutaneous coronary intervention (PPCI) to non-diabetic patients.
Methods
240 non-diabetic patients with STEMI were recruited and underwent PPCI. After revascularization, epicardial reperfusion had been assessed by Thrombolysis in myocardial infarction (TIMI) flow grades (TFG) and TIMI frame count (TFC), and myocardial reperfusion had been assessed by TIMI myocardial perfusion grade (TMP) and ST-segment resolution (STR). NAFLD had been assessed and graded based on abdominal ultrasonography then the patients were subdivided into; NAFLD group (111 patients) and non-NAFLD group (129 patients).
Results
The overall prevalence of NAFLD in the current study was 46.5%. Clinically, KILLIP class > I was significant in NAFLD group (24 (P< 0.001). Multi-vessel coronary artery disease (CAD) was significant in NAFLD group (63 (56.8%) vs. 23 (17.8%); P< 0.001). Eleven patients of NAFLD group died with no deaths occurred in the other group. Post-procedural myocardial blush grade (MBG) zero and 1 were significant in patients with NAFLD group (P< 0.001). Also, absent STR and TFC were significant (P< 0.001) in NAFLD group. Finally, NAFLD was an independent predictor for in-hospital and follow up cardiac events.
Conclusions
NAFLD is considered an independent risk factor for the occurrence of in-hospital and …
Dietary pattern of patients with type 2 diabetes and hyperlipidemia
Vocal Dysfunction Following Thyroid Surgery: A Multidimensional Subjective and Objective Study
Background and objective: Following thyroid surgery, vocal changes are a common complication and well-known morbidity that may be linked to neuronal and nonneuronal voice breakdown. Nevertheless, their effects on different voice characteristics are not fully understood, and their bases are still poorly characterized. In order to determine the diagnostic indicators that address the nature of such post-thyroidectomy voice alternations, this study was designed to provide a multidimensional assessment of vocal function after thyroid surgery. Methods: This research was a one year prospective cohort study conducted on 100 adult patients aged 40.19 (±12.82) years who were recruited from the outpatient clinic of Phoniatric Unit, Assiut University Hospital and scheduled to undergoing thyroid surgery during the period from November 2020 to November 2021. All subjects underwent vocal assessment preoperatively, 15-days, 1 month and 2 months postoperatively by filled in subjective evaluation of voice complaints via voice handicap index (VHI-30), auditory perceptual assessment (APA) of the voice, videolaryngoscopy in addition to acoustic analysis using computerized speech lab (CSL). Statistical analysis was performed to comparing multi-parameters voice assessment tools across different assessment time points. Results: The voice changes were significantly decreased from 51.0% after 15 days postoperatively to 33.0% after 2 months of follow up. Among these cases, 35.0% cases developed vocal fold paralysis and complained of a breathy voice (27% developed unilateral vocal fold paralysis, and 8% developed bilateral focal fold lesions) and the remaining 16.0% cases had no paralytic manifestations. Also, only one case developed gross lesion “bilateral vocal fold nodules”. The subjective evaluation of voice outcome after thyroidectomy showed significant improvement in VHI subscales and total score from 15 days postoperatively to two months of follow up (P<0.001). All of the acoustic parameters except HNR showed a significant difference across the different assessment settings (P<0.001). Conclusion: Thyroidectomy can result in significant vocal alterations, even in cases where the laryngeal nerve is unharmed. These changes should be taken into consideration in patient having thyroid surgery, especially a total thyroidectomy because of malignant lesions. More efforts are needed in order to determine the extent and pathophysiological reasons for the vocal alterations following thyroid surgery in order to reduce the morbidity associated with one of the most popular surgical procedures performed globally.
Regarding the research advice request form
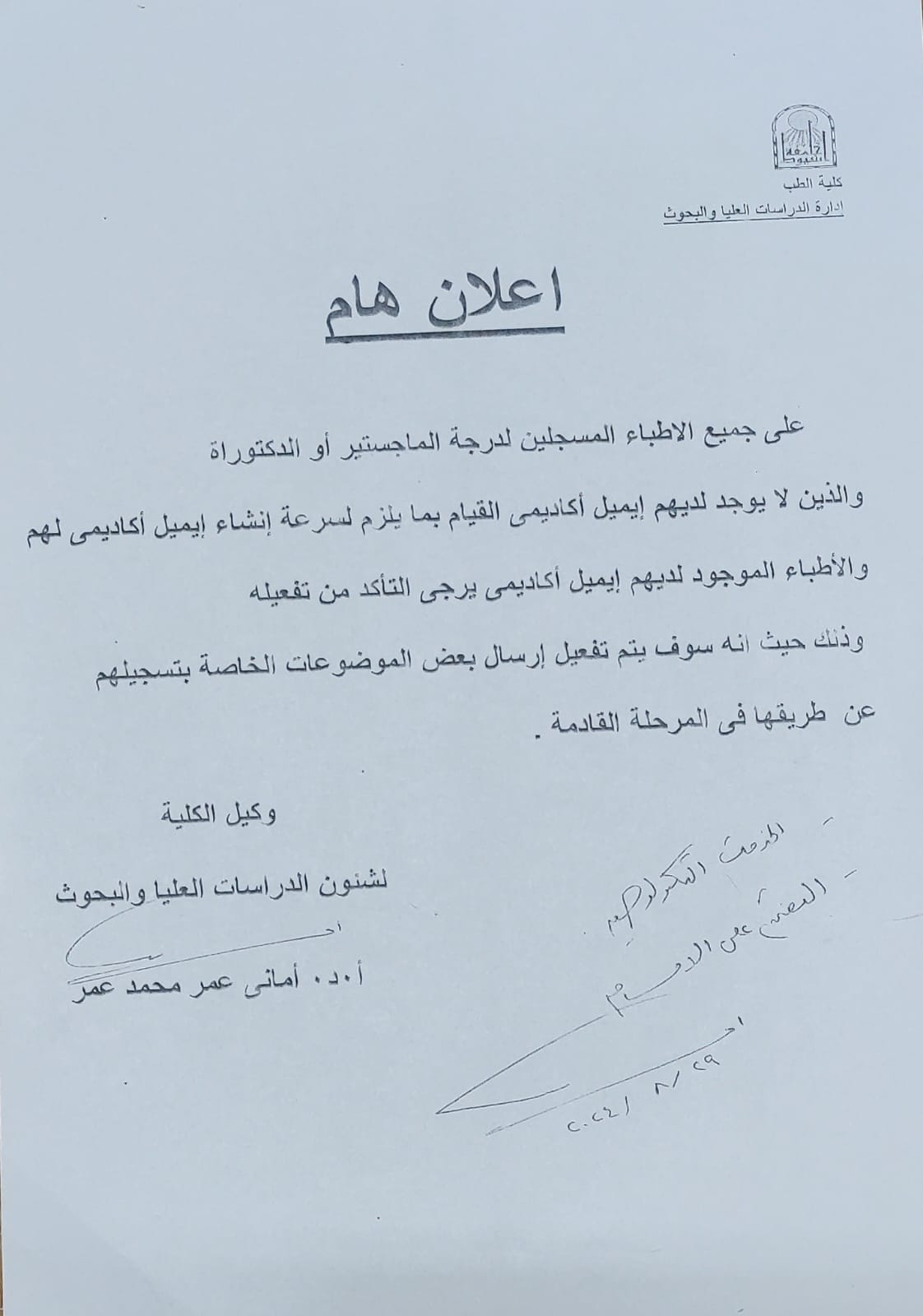
Regarding creating an academic email and ensuring its activation
 Do you have any questions?
Do you have any questions? 

